Diabetes mellitus is a metabolic disorder owing to the poor regulation of blood glucose. This might influence various organs (heart, vascular, eye, neuron) and lead to numerous life-threatening complications or even death. Prolonged postprandial blood glucose levels (hyperglycemia) are one of the major independent risk factors for developing type 2 diabetes (T2DM). Hyperglycemia is the result of impaired glucose regulation including reduced insulin secretion, decreased glucose utilization, and increased glucose production. Insulin is the most important regulator of glucose homeostasis. Peripheral insulin resistance and abnormal insulin secretion leads to hyperglycemia, brain insulin resistance is associated with neuronal dysfunction and cognitive impairment in Alzheimer’s dementia. People with postprandial hyperglycemia, pancreatic β-cells decline insulin secretion after food ingestion and glucagon release is less inhibited. Thus, more glucose enters the circulation, which leads to prolonged plasma glucose increases. Glucose homeostasis is shown in Fig. 1.
    |
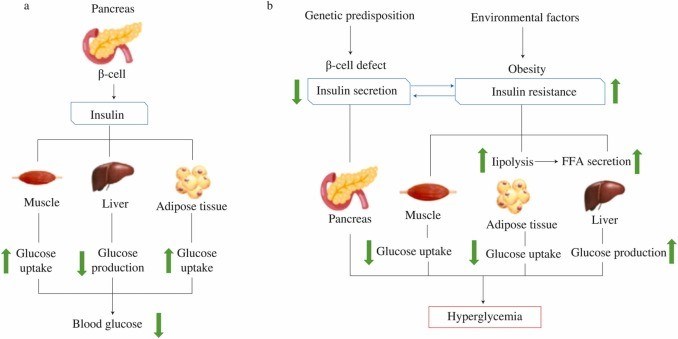 |
| Fig. 1 Glucose homeostasis. (a) Normal function of insulin pathway when balancing hepatic glucose production and peripheral glucose uptake and utilization - after meal, when the blood glucose level is high, insulin is released from the pancreatic β-cells to stimulate glucose uptake in the muscle and adipose tissues and promote glycogenesis in the liver. (b) Hyperglycemia displays when insulin secretion cannot offset insulin resistance. Skeletal muscle, liver, and adipose tissues primarily demonstrate insulin resistance. The insulin resistance promotes impaired glucose uptake into skeletal muscle and impaired inhibition of glucose production in the liver, with following increases in blood glucose levels. In the adipocytes are disturbed lipolysis and enhanced delivery of free fatty acids. Fatty acids accumulate in the skeletal muscle, liver, and pancreas and promote insulin resistance, raised hepatic glucose production, and impaired β-cell function. |
Phenolics compounds can be divided into flavonoids and non-flavanoid groups. Flavonoids are consisting of six groups: flavonols, flavones, flavan-3-ols, flavanones, isoflavonoids, and anthocyanins. The major non-flavonoids are phenolic acids, stilbenes, lignans, and tannins. The most potential polyphenols from functional foods that can induce hypoglycemic effects across different hyperglycemic pathological pathways (Fig. 2).
    |
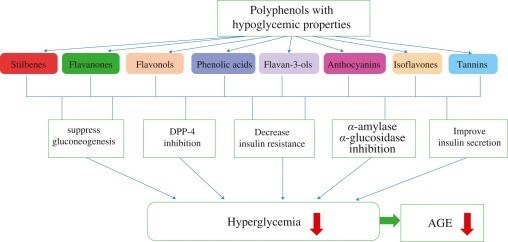 |
| Fig. 2 Polyphenols and their hypoglycemic pathways of hyperglycemia |
Flavanones-naringin and hesperidin (Fig. 3) present in fruits and vegetables exhibit anti-diabetic activity, promote glycogen synthesis, and reduce expression of phosphoenolpyruvate carboxykinase (PEPCK) and glucose-6-phosphatase (G6P), thereby repressing gluconeogenesis. Additionally, hesperidin strongly inhibits the enzyme DPP-4.
Flavonol-quercetin (Fig. 4a) is a compound in onions, apples, and berries. Quercetin from berry improves glucose uptake in myoblasts, enhances insulin sensitivity by activating the AMPK-signaling pathway, and also improves insulin resistance in hepatic cells. Moreover, quercetin shows high suppression of α-glucosidase, stimulates insulin secretion by increasing Ca2+ influx, and has anti-glycation properties.
    |
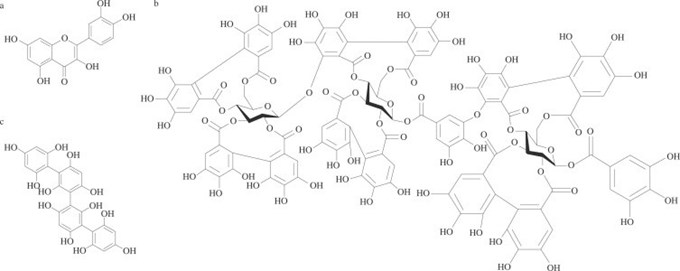 |
| Fig. 4 Chemical structure of (a) quercetin, (b) ellagitannin, (c) phlorotannin. |
Tannins such as hydrolyzable tannins (ellagitannins) (Fig. 4b) from berries exhibit inhibition of α-amylase [38], while phlorotannins of algae inhibit the activities of α-glucosidase and α-amylase, improving postprandial hyperglycemia, and insulin sensitivity (Fig. 4c). Persimmon tannin suppresses α-glucosidase and reduces postprandial blood glucose levels.
Flavan-3-ols include epigallocatechin gallate (EGCG), (+)-catechin, (−)-epicatechin, and proanthocyanidins (procyanidin B2) (Fig. 5). Procyanidin B2, (−)-epicatechin, and (+)-catechin apple, cinnamon, grape and chocolate significantly reduced insulin resistance in T2DM subjects [42-45]. EGCG in green tea lowered insulin resistance, improved glucose uptake. Moreover, EGCG decreases glucose production by inhibiting the expression of PEPCK and G6P. Proanthocyanidins (cacao, black soybean seed coat, grape seeds) improve glucose uptake and limit glucose output, raising hepatic glucokinase activity in vitro studies. Moreover, proanthocyanidins reduce G6P.
    |
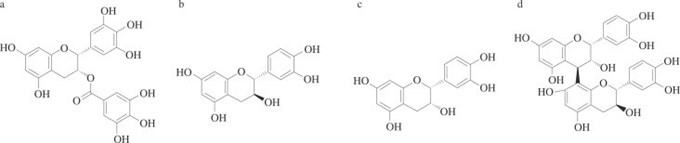 |
| Fig. 5 Chemical structure of (a) EGCG, (b) (+)-catechin, (c) (−)-epicatechin, (d) procyanidin B2. |
Soy isoflavonoids: genistein and daidzein (Fig. 6) increases insulin sensitivity and glucose uptake into muscles. Furthermore, isoflavonoids improves β-cell function and insulin secretion.
    |
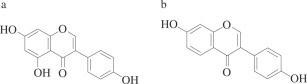 |
| Fig. 6 Chemical structure of (a) genistein, (b) daidzein. |
Resveratrol (Fig. 7a) significantly reduced blood glucose, lowered hepatic gluconeogenic enzyme activity, and hepatic glycogen in mice
    |
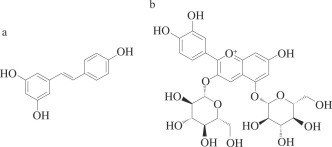 |
| Fig. 7 Chemical structure of (a) resveratrol, (b) cyanidin-3,5-O-diglucoside |
Anthocyanins from berries increase glucose uptake, improve insulin sensitivity, and enhance insulin release from pancreatic β-cells, improve insulin resistance in vivo study. Moreover, anthocyanins act as α-glucosidase inhibitors. Anthocyanins from black bean and cyanidin-3,5-O-diglucoside (aronia juice) exhibit inhibition on DPP-4. Anthocyanins from purple potato stimulated insulin secretion in mouse beta cells.
Phenolic acids include chlorogenic acid, ferulic acid, p-coumaric acid, quinic acid, cinnamic acid and vanillic acid (Fig. 8). Phenolic acids are present in fruits, vegetables, spices, berries and grains
Coffee chlorogenic acid improves hyperglycemia, insulin resistance and lowers the glucose absorption. Ferulic and p-coumaric acids from whole cereals suppress α-glucosidase [35,69]. Moreover, ferulic acid improves insulin sensitivity and hepatic glycogenesis but inhibits gluconeogenesis in type 2 diabetic rats. Cinnamic, quinic and vanillic acid significantly enhanced glucose-stimulated insulin secretion