1. Introduction
Health effects of trans fatty acids (TFAs) on human organisms can vary according to their type, structure, composition, and origin
Dietary fats, including TFAs, have been one of the central topics of discussion in scientific literature and have received more attention from health professionals and the public than any other nutrients in the food supply [1]. TFAs are unsaturated fatty acids containing at least one double bond in its trans configuration [2]. Trans fat is the final product of a chemical process called partial hydrogenation of cis-unsaturated fatty acids.
Overall, there are four main sources of TFAs in the human diet; industrially produced TFAs by partial hydrogenation of vegetable oils, TFAs produced during heat processes, TFAs occurring naturally in ruminant sources, as well as TFAs synthesized for utilization as dietary supplements [3]. TFAs are classified according to the two main sources they come from, “industrial” and “natural”. Industrial or artificial TFAs are produced during manufacturing by partial hydrogenation of liquid vegetable or fish oils containing unsaturated fatty acids. On the other hand, nTFAs are produced in the rumen of ruminant animals like cows, sheep, and goats by bacterial transformation of unsaturated fatty acids derived from feed. A small amount of TFAs is also present in poultry and pork fat [4,5].
    |
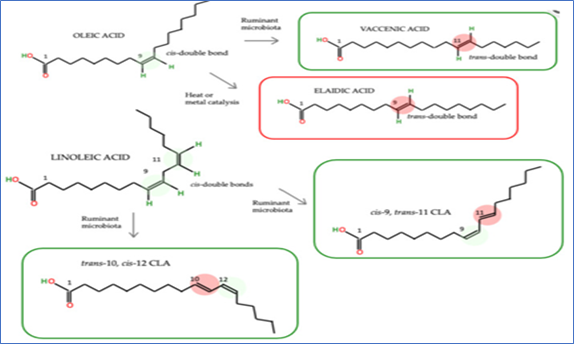 |
| Chemical structure of the major TFA in the green box are nTFA |
2. Health Effects of TFAs
2.1 Obesity
Different data were found in relation to iTFAs, where a positive correlation between iTFA consumption and obesity was found. In the EPIC-PANACEA (Physical Activity, Nutrition, Alcohol, Cessation of Smoking, Eating out of Home, and Obesity) study, the doubling of elaidic acid was associated with a decreased risk of weight loss [7]. In the Spanish INMA (INfancia y Medio Ambiente) study similar results were found in 4- to 5-year-old children. Indeed, iTFA intake of >0.7 g/day was positively associated with being overweight, including obesity; differently, in the same study, no significant association for nTFAs was found [8]. The same results were confirmed in the cross-sectional study of Honicky and colleagues on children and adolescents who underwent a procedure to treat congenital heart disease. In this study, the patients that exceeded the iTFA intake recommendation of 1% of energy had a 5-fold increase of central adiposity [9]. Some recent explanations have related the iTFA consumption with the increased genetic susceptibility of the obesity-associated gene polymorphisms (rs1121980, rs1421085, and rs8050136) and BMI or weight changes, highlighting the important role that iTFAs can have on human metabolism [10].
2.2. Cardiovascular Disease (CVD)
There are numerous studies providing evidence that iTFAs increase the risk of coronary heart disease [11]. It has been stated that TFA consumption perturbs the body’s ability to metabolize essential fatty acids (including omega-3 fatty acids) leading to changes in the phospholipid fatty acid composition in the aorta, thus increasing the CVD risk [12]
2.3. Cancer
There is a positive relationship between TFA intake and the incidence of breast and large intestine cancer [13]. Similarly, more recently, Ardisson Korat and colleagues [14] found a positive relationship between TFA levels in red blood cell membrane and the risk of large B cell lymphoma, especially for elaidic and vaccenic acid [14]. Matta et al. [15] support the hypothesis that higher dietary intakes of iTFAs, in particular elaidic acid, are associated with elevated breast cancer risk.
References
1. Semma M. Trans Fatty Acids: Properties, Benefits and Risks. J. Health Sci. 2002;48:7–13. doi: 10.1248/jhs.48.
2. European Food Safety Autority (EFSA) Opinion of the Scientific Panel on Dietetic products, nutrition and allergies [NDA] related to the presence of trans fatty acids in foods and the effect on human health of the consumption of trans fatty acids. EFSA J. 2004;2:1–49. doi: 10.2903/j.efsa.2004.81
3. Aldai N., de Renobales M., Barron L.J.R., Kramer J.K.G. What are the trans fatty acids issues in foods after discontinuation of industrially produced trans fats? Ruminant products, vegetable oils, and synthetic supplements. Eur. J. Lipid Sci. Technol. 2013;115:1378–1401. doi: 10.1002/ejlt.201300072
4. Valenzuela C.A., Baker E.J., Miles E.A., Calder P.C. Eighteen-carbon trans fatty acids and inflammation in the context of atherosclerosis. Prog. Lipid Res. 2019;76 doi: 10.1016/j.plipres.2019.101009
5. Wanders A.J., Zock P.L., Brouwer I.A. Trans fat intake and its dietary sources in general populations worldwide: A systematic review. Nutrients. 2017;9:840. doi: 10.3390/nu9080840
6. Chajès V., Biessy C., Ferrari P., Romieu I., Freisling H., Huybrechts I., Scalbert A., Bueno de Mesquita B., Romaguera D., Gunter M.J., et al. Plasma Elaidic Acid Level as Biomarker of Industrial Trans Fatty Acids and Risk of Weight Change: Report from the EPIC Study. PLoS ONE. 2015;10:e0118206. doi: 10.1371/journal.pone.0118206
7. Chajès V., Biessy C., Ferrari P., Romieu I., Freisling H., Huybrechts I., Scalbert A., Bueno de Mesquita B., Romaguera D., Gunter M.J., et al. Plasma Elaidic Acid Level as Biomarker of Industrial Trans Fatty Acids and Risk of Weight Change: Report from the EPIC Study. PLoS ONE. 2015;10:e0118206. doi: 10.1371/journal.pone.0118206.
8. Scholz A., Navarrete-Muñoz E.M., García-de-la-Hera M., Fernandez-Somoano A., Tardon A., Santa-Marina L., Pereda-Pereda E., Romaguera D., Guxens M., Beneito A., et al. Association between Trans Fatty Acid Intake and Overweight Including Obesity in 4 to 5-year-old Children from the INMA Study. Pediatr. Obes. 2019;14:e12528. doi: 10.1111/ijpo.12528.
9. Honicky M., Cardoso S.M., Lima L.R.A., Ozcariz S.G.I., Vieira F.G.K., Carlos Back I., Moreno Y.M.F. Added Sugar and Trans Fatty Acid Intake and Sedentary Behavior Were Associated with Excess Total-body and Central Adiposity in Children and Adolescents with Congenital Heart Disease. Pediatr. Obes. 2020;15:e12623. doi: 10.1111/ijpo.12623
10. Koochakpour G., Esfandiar Z., Hosseini-Esfahani F., Mirmiran P., Daneshpour M.S., Sedaghati-Khayat B., Azizi F. Evaluating the Interaction of Common FTO Genetic Variants, Added Sugar, and Trans-Fatty Acid Intakes in Altering Obesity Phenotypes. Nutr. Metab. Cardiovasc. Dis. 2019;29:474–480. doi: 10.1016/j.numecd.2019.01.005
11. Micha R., Mozaffarian D. Trans fatty acids: Effects on cardiometabolic health and implications for policy. Prostaglandins Leukot. Essent. Fat. Acids. 2008;79:147–152. doi: 10.1016/j.plefa.2008.09.008
12. Kummerow F.A., Zhou Q., Mahfouz M.M., Smiricky M.R., Grieshop C.M., Schaeffer D.J. Trans fatty acids in hydrogenated fat inhibited the synthesis of the polyunsaturated fatty acids in the phospholipid of arterial cells. Life Sci. 2004;74:2707–2723. doi: 10.1016/j.lfs.2003.10.013
13. Stender S., Dyerberg J. Influence of trans fatty acids on health. Ann. Nutr. Metab. 2004;48:61–66. doi: 10.1159/000075591
14. Ardisson Korat A.V., Chiu Y.H., Bertrand K.A., Zhang S., Epstein M.M., Rosner B.A., Chiuve S., Campos H., Giovannucci E.L., Chavarro J.E., et al. Red blood cell membrane trans fatty acid levels and risk of non-Hodgkin lymphoma: A prospective nested case-control study. Am. J. Clin. Nutr. 2020;112:1576–1583. doi: 10.1093/ajcn/nqaa251
15. Matta M., Huybrechts I., Biessy C., Casagrande C., Yammine S., Agnès Fournier A., Olsen K.S., Lukic M., Gram I.T., Ardanaz E., et al. Dietary intake of trans fatty acids and breast cancer risk in 9 European countries. BMC Med. 2021;19:81. doi: 10.1186/s12916-021-01952-3.